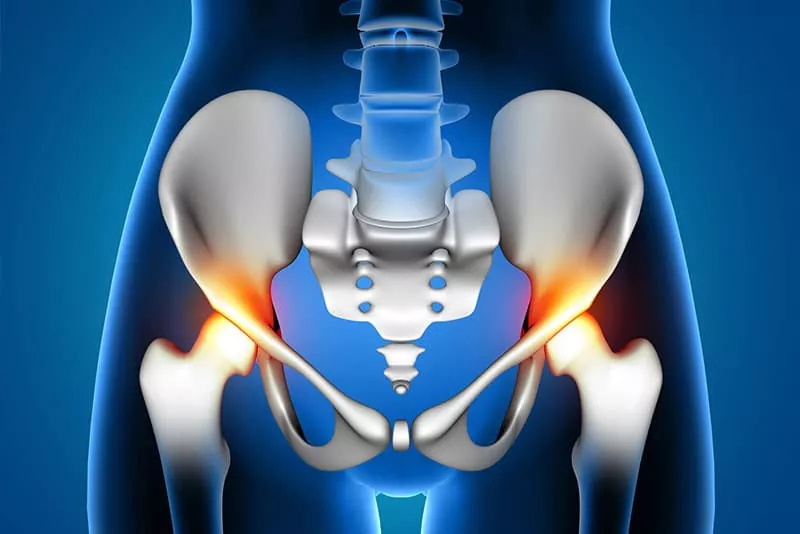
Direct Anterior (DA) Hip Replacement Surgery

Direct anterior hip replacement offers an exciting less invasive alternative to traditional techniques used to perform hip arthroplasty. This technique is the only way to access the hip joint that is truly muscle sparing, making it the least invasive of all techniques used to access the hip. The traditional posterior approach requires the surgeon to split the gluteus maximus, which is one of the largest muscles in the lower extremity, and to release several of the short rotators of the hip.
The unique advantage of the direct anterior approach is the ability to access the hip joint, by using a truly intermuscular plane. The interval between the Sartorius and the Tensor Fascia Lata muscles is used to expose the hip capsule. Using a truly intermuscular interval, the surgeon does not need to “cut, split, or release” any of your muscles. The anterior approach allows the surgeon to minimize the trauma to the muscles while accessing the hip joint. This translates into decreased inflammation, less pain, quicker return to function, and much less restrictive precautions after surgery.
The posterior approach requires more restrictive post-operative hip precautions. The anterior approach is inherently more stable – allowing patients much more liberal precautions and quicker return to normal daily activities. With the anterior approach, the patient may reach over to tie their shoes, squat to low levels, sit on standard toilet seats, and there is no need for pillows between the legs or restrictive sleeping positions.
The anterior approach is performed with the patient flat on their back and an x-ray machine is used in surgery to verify the position of the implants during surgery. A special table is used to position and manipulate the patient’s legs in the operation. This allows the surgeon to judge the position of the components and to ensure that leg lengths and hip offset are recreated as precisely as possible. Standard posterior hip surgery is performed with the patient in the lateral (sideways) position.
With less muscle dissection in surgery, the anterior approach allows the patient the advantage of less pain, quicker return to normal gait, faster return to physical work, simpler restrictions after surgery.
The anterior approach allows for many advantages to the patient. However, not all patients are ideal candidates for this procedure. It is important that the patient and surgeon discuss unique patient risk factors.
The anterior approach also has several unique risks associated with the procedure. There is a small sensory nerve (lateral femoral cutaneous nerve), on the outside of the thigh. This nerve may become irritated or stretched in the surgery resulting in a small numb spot on the side of the thigh that is usually temporary. The femoral stem is also slightly more difficult to place in the direct anterior hip arthroplasty. Special anatomical stems and instruments have been developed to help surgeons perform anterior hip replacement. Despite these advancements, there is a slightly higher incidence of femoral fracture and stem loosening in the anterior approach compared to the posterior approach. Therefore, patients with osteoporosis may benefit from the utilization of bone cement to anchor the stem in the femur.
Although anterior hip arthroplasty is an exciting alternative to traditional exposures to the hip, hip replacement surgery is a very reliable and reproducible operation for relieving arthritis and other types of intractable hip pain.
Modern surgical techniques and highly advanced surgical pathways have offered many substantial improvements in the recovery time and expected outcomes after hip surgery. Surgical procedures are commonly performed under regional anesthesia, like a spinal. Local anesthesia is infiltrated in the soft tissues around the hip and a multi-modal pain management strategy allows for early ambulation and very limited hospital stays.
Most patients can expect to spend 24 hours or less in the hospital after a successful surgical procedure. Physical therapists evaluate patients immediately after surgery with immediate weight bearing and early ambulation. Most patients can walk several hundred feet with a walker or cane immediately after surgery. Modern surgical techniques have significantly reduced the requirement for blood transfusions after hip replacement surgery.
After discharge from the hospital, most patients are able to ambulate fairly independently with use from an assistive device (cane or walker). Outpatient physical therapy (out of the house) is prescribed for 2-3 visits per week for 4-8 weeks to regain strength, balance, and endurance. Most patients can expect to return for follow up at 3-4 weeks from surgery with limited or no assistance from a walker or cane.
It is reasonable to expect to return to office work in 2-4 weeks, and physical labor in 8-12 weeks. Recreational sports such as golf, tennis, or swimming can be enjoyed in 6-8 weeks after hip replacement surgery.
An important predictor of post operative recovery is pre-operative physical fitness and conditioning. Every patient has a unique recovery trajectory and must be managed on a personal basis with individual recovery goals and milestones.